Introduction: Why It’s Important to Know the Difference
Fatty liver is an increasingly observed medical problem worldwide. It has two main forms: alcoholic fatty liver disease and non-alcoholic fatty liver disease. Both diseases result in abnormal fat deposition within the liver; however, they differ mainly in the causes and risk factors.
Knowing these differences will help in creating awareness so as to prevent and manage the disorder. This article will discuss and compare the major differences between the two diseases, including the causes, symptoms, treatment options of fatty liver disease, and how to maintain a healthy liver for a healthier lifestyle.
What Is Alcoholic Fatty Liver Disease (AFLD)?
Alcoholic Fatty Liver Disease (AFLD) is a liver disorder occurring from excessive or long-term alcohol consumption that brings upon fat deposits in the liver cells. Generally, the liver breaks down fats, but alcohol inhibits the process, so abnormal fat is deposited.
In the duration of the early phase of AFLD, one might not have any symptoms, with the liver continuing to sustain damage with alcoholic hepatitis, fibrosis, or cirrhosis developing later if drinking continues. But the liver will often be able to heal and recover if caught in time, and alcohol intake is stopped completely.
You Can Also Read:- Thyroid Disease: What It Is, Causes, Symptoms & Treatment
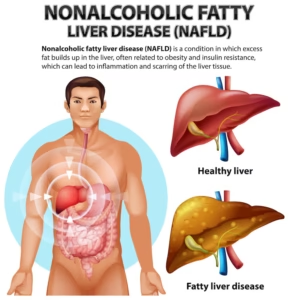
What Is Non-Alcoholic Fatty Liver Disease (NAFLD)?

Some amount of fat is deposited in the liver in this particular condition in individuals who consume little or no alcohol. It is important to note the key difference between the two possibilities, NAFLD and alcoholic fatty liver disease, since NAFLD is mainly linked to metabolic factors such as obesity, type 2 diabetes mellitus, high cholesterol, and a sedentary lifestyle.
During its early course, the disease may not present any clear-cut symptom, but it silently damages the liver and evolves into severe stages like non-alcoholic steatohepatitis (NASH) or fibrosis or cirrhosis. In cases of early diagnosis and proper lifestyle changes: weight loss, improved diet, and increased exercise, it is very possible to reverse NAFLD and restore liver health.
What is the difference between alcoholic vs. non-alcoholic fatty liver?

The following table provides a clear comparison between AFLD and NAFLD:
| Aspect | Alcoholic Fatty Liver Disease (AFLD) | Non-Alcoholic Fatty Liver Disease (NAFLD) |
| Cause | Caused by excessive and long-term alcohol consumption. | Due to metabolic factors like obesity, type 2 diabetes, high cholesterol, and lack of exercise. |
| Risk Factors | Mainly affects individuals with a history of heavy drinking. | Common in people with obesity, diabetes, high blood pressure, or high cholesterol, even with little or no alcohol use. |
| Symptoms | May include fatigue, jaundice, abdominal discomfort, and alcohol-related health issues. | Early phases are likely to be asymptomatic but may involve fatigue, mild abdominal pain, or metabolic disturbances. |
| Progression | It can lead to alcoholic hepatitis, fibrosis, or cirrhosis with the continued ingestion of alcohol. | Might lead to non-alcoholic steatohepatitis (NASH), fibrosis, or cirrhosis if lifestyle and metabolic problems are left unattended. |
| Treatment | Primary treatment is complete abstinence from alcohol along with a healthy diet and medical care. | Treatment focuses on lifestyle modifications such as weight loss, a balanced diet, exercise, and managing underlying health conditions. |
How is Fatty Liver Diagnosed?
A diagnosis of fatty liver is carried out by various medical approaches that assist in detecting fat accumulation and checking the general health of the liver. The chief diagnostic tests include:
- Physical Examination & History: The physician first investigates the patient’s lifestyle factors and alcohol use, family history, etc., while checking signs of obesity or hepatomegaly.
- Blood Investigations: Similarly, liver function tests are conducted to check if enzyme levels like ALT and AST are raised, which might provide an indication of liver injury.
- Ultrasound or Imaging Scans: Non-invasive investigations may include ultrasound, CT scan, or MRI to see if there are any fat deposits in the liver.
- Fibroscan Evaluation: It is a further advanced ultrasound evaluation of fat content and liver stiffness to determine the degree of fibrosis.
- Liver Biopsy Confirmation: In a few cases, such as the need for greater clarity, a biopsy will be performed to analyze liver tissue and confirm the extent of fatty changes and damage.
You Can Also Read:- Irregular Periods: What Your Body Is Trying to Tell You
What are the treatments for Alcoholic and Non-Alcoholic Fatty Liver?

Treatment for AFLD or NAFLD primarily aims at addressing the main causative agent, reversing damage to the liver, and preventing progression to cataclysmic consequences such as cirrhosis. There is a tweak or two in the treatment of AFLD and NAFLD; however, lifestyle and medical guidance remain common to both. These are:
- Alcohol Abstinence (AFLD): In alcohol-induced fatty liver, the single most successful intervention is abstinence from alcohol, with simultaneous healing of the liver. Once abstinence begins, no further damage occurs.
- Lifestyle Modification (NAFLD): Lifestyle measures are all the treatments for NAFLD. Targets for lifestyle change include maintaining normal weight, regular exercise, and proper diet.
- Medication and Treatment of Associated Disorders: There is no medication currently used for fatty liver per se; however, by treating associated conditions such as diabetes, hypercholesterolemia, and hypertension, one may prevent the progression of the fatty liver.
- Nutritional Support: Foods that support liver recovery are fresh fruits and vegetables, whole grains, lean proteins, and healthy fats. Avoid processed food, sugary drinks, and excess fats.
- Continual Monitoring of Cases: Follow-up examinations and use of blood tests or imaging procedures to track the liver condition allow early recognition of any complications and their management.
- Additional Liver Health Tips: Being well hydrated is the greatest; in addition, hold any alcohol or medications unless that medication is prescribed especially for this condition by an actual health care provider. Find time to relax, and follow lifestyle tips as given by your doctor.
How can Fatty Liver Be Reversed?
Fatty liver disease is reversible in the early stage with consistent lifestyle modifications and medical interventions; in short, reducing fat accumulation in the liver and managing the causes. The main ways that pose the possibility of reversing fatty liver are:
- Complete Avoidance of Alcohol: The most crucial measure is to stop drinking alcohol completely with alcoholic fatty liver disease so the liver can heal and not suffer any further damage.
- Weight Loss: Shedding excess weight gradually through diet and exercise can decrease fat in the liver, particularly in non-alcoholic fatty liver disease.
- Proper Diet: Eating a variety of foods rich in nutrients including vegetables, fruits, lean proteins, whole grains, and healthy fats; however, it is worth noting that processed foods, added sugars, and fried foods are something we should avoid if we want to support the recuperating process of the liver.
- Exercise: Exercising at least 30 minutes per day, most days of the week, may enhance metabolism, reduce liver fat, and improve general health.
- In proper management, one controls diabetes, blood pressure, and cholesterol with adequate treatment and medication to reduce the chances for fatty liver to worsen.
- Routine Monitoring and Assessments: Regular check-ups with liver function test and imaging investigations will help to monitor improvement and keep the reversal process on track.
How to Keep Your Liver Healthy: Tips?
Here are some tips that lead to a better and healthier Liver, which will help to resist the fat accumulation on it.
- Eat Liver-Friendly Foods: Enrich your dish with items packed with antioxidants such as spinach, garlic, turmeric, walnuts, and beetroot, all of which promote liver detoxification.
- Try Some Simple Home Remedies: The natural ways to keep your liver healthy include drinking warm lemon water in the morning, green tea during the day, and aloe vera occasionally.
- Avoid Bad Foods: Minimize sugary drinks, fried snacks, and refined carbohydrates responsible for fatty deposits.
- Keep Yourself Hydrated: About 3 liters of water should be drunk to flush out toxins and aid the liver to function smoothly.
- Cardio Exercises: At least 30–40 minutes of brisk walking, jogging, cycling, or swimming, five days a week will aid the metabolism and curb further fat production in the liver.
- Strength Training: Performing squats, push-ups, and planks two to three times a week helps the liver instead of making it fatty changes due to response.
When to See a Doctor?
Typically silent, the fatty liver disease can harbor the very real danger of advancing into severe liver damage; therefore, knowing when to visit a doctor can provide immense opportunity to prevent further impairments. If you are experiencing any of the following symptoms or risk factors, speak with your physician:
- Persistent Weakness and Fatigue: If you experience an unexplained weakness or fatigue, it could be a sign of liver dysfunction.
- Abdominal Pain or Discomfort: Pain or a feeling of heaviness in the right upper abdominal region may indicate inflammation and an enlarged liver.
- An Unexplained Loss of Weight or Appetite: A sudden change in appetite or weight typically indicates that there is a problem with the liver.
- Jaundice: It chills down your heartbeat to realize that yellowness of skin or eyes is a very serious warning sign of liver damage, demanding immediate medical care.
- Dark Urine or Pale Stools: With such peculiar changes in the color of urine and stools, bile flow and liver function may be under question.
- Swelling in Legs or Abdomen: Accumulated fluid called edema (in the legs) or ascites (in the abdomen) can be an indication of advanced liver disease.
Conclusion
To conclude, alcoholic fatty liver disease and non-alcoholic fatty liver disease require timely treatment to prevent vital liver disorders. If patients get certain fatty liver causes, signs of fatty liver, and the right fatty liver treatment, they usually give the ailment a retrograde and preserve their well-being.
Easy lifestyle changes such as partaking in exercise, eating the right kind of foods, and providing for proper liver health play a level of essentiality in recovery. Since fatty liver falls in the division of Gastroenterology and Hepatology, consulting a specialist becomes imperative. Shekhawati Hospital stands distinguished with contemporary technologies and highly competent experts for deeper liver treatment.